|
The calculation of SAR in human subjects is very complex (and imprecise), requiring sophisticated mathematical modeling and computer simulations. All commercially available MR scanners have programs that estimate SAR values automatically when a specific imaging protocol is selected and warn the operator if regulatory limits are likely to be exceeded. However, each manufacturer uses a different proprietary algorithm, so calculated SAR values may differ substantially among vendors. SAR estimation also requires an accurate patient weight to be input by the technologist (although most modern scanners also monitor transmitted power to prevent excessive RF exposure if an incorrect weight has been entered).
|
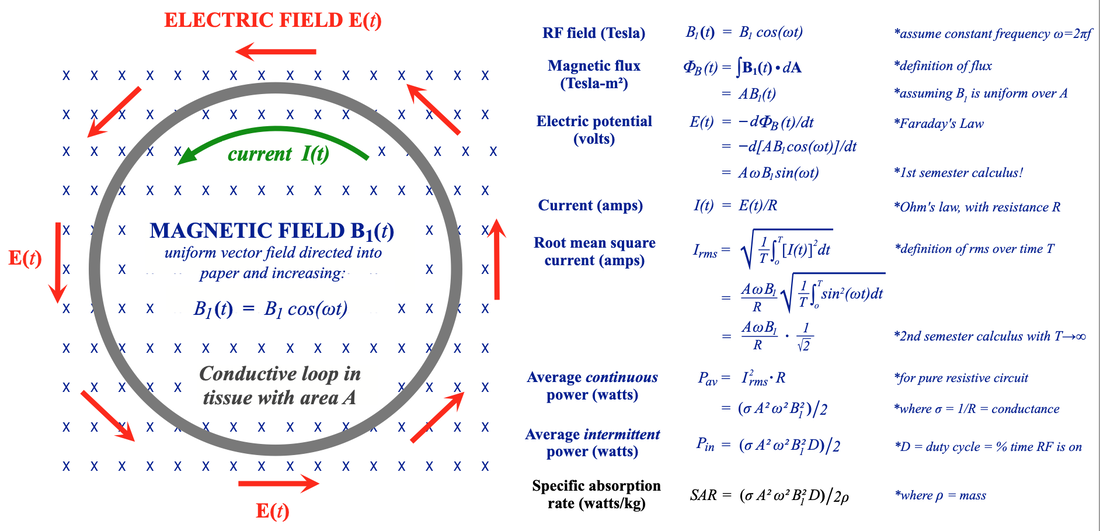

- SAR is proportional to the electrical conductivity of tissue (σ). Tissue conductivity varies by a factor of 10 across the body, being largest in high water content materials like blood and urine and lowest in tissues like bone, fat, and lung. Foreign metal objects in the body are frequently highly conductive and significant (even dangerous) heating levels around these may occur.
- SAR increases significantly with body size. In our 2-dimensional model we found SAR proportional to A², the square of the body cross-sectional area. Because A = πr² (where r is the radius), our model predicts SAR proportional to r4. When the third dimension is considered, SAR actually proves to be more closely proportional to r5. SAR tends to be concentrated more around the periphery (where the radius is larger). So larger and obese patients are more at risk. In a homogeneous sphere, 87% of the RF power dissipation occurs in its the outer third. Even in inhomogeneous humans, the peripheral deposition of heat can be appreciated in the SAR map above. Fortunately heat deposited on the perimeter of the body can be more easily dissipated.
- SAR is proportional to the square of the RF frequency (ω). Typically, the RF frequency is chosen to closely match the Larmor frequency, which, in turn, is directly proportional to static field strength Bo. So, all other things being equal, SAR depends on the square of Bo. The same pulse sequence in the same patient imaged at 1.5T would therefore generate 4x the SAR if performed at 3.0T.
- SAR is proportional to the square of the RF-flip angle (α). This follows from the fact that (α) is proportional to the mean amplitude of the RF-pulse (B1). Since SAR is proportional to B1², it is also proportional to α². Thus a 180º-pulse would create 4x the SAR as a 90º-pulse.
- SAR is proportional to the duty cycle (D). Duty cycle represents the percent time in a pulse sequence RF is being transmitted. Thus more intense sequences (with lots of RF pulses applied in a short period of time) generate high levels of SAR.
Although SAR is the dominant source of tissue heating, it is only one determinant of tissue temperature. Other critical factors include: regional perfusion, baseline patient body temperature, the patient's thermoregulatory capacity, ambient temperature, airflow through the scanner bore, relative humidity, clothing, and ability to perspire. Patients at risk for overheating include those with reduced thermoregulatory capacities — infants, pregnant women, the elderly, obese, diabetics, febrile patients, and those with cardiac decompensation. Certain medications — including beta-blockers, diuretics, calcium-channel blockers, amphetamines, and sedatives — can also impair thermoregulatory responses. These factors should always be considered when scanning a susceptible patient, even if predicted SAR values seem to be within tolerable limits.
Advanced Discussion (show/hide)»
Displacement Current Considerations
One of the important factors left out of our simple SAR model above is considering the electromagnetic effects of the induced circulating current I(t). According to Ampere’s Law, this current also creates its own magnetic field defined by the so-called displacement current (JD), which, in turn, induces a new field (BD(t)), that combines with the original source field (B1(t)). When this new induced field is considered, it means that the effective electric field within the tissue is no longer a simple function of the initial amplitude of B1(t). This effect becomes increasingly important at higher magnetic fields and must be incorporated into sophisticated models for SAR.
Methods for Measuring SAR
The National Electrical Manufacturers Association (NEMA) has developed guidelines for measuring SAR generated by equipment using phantoms, incorporated in their standard MS 8-2016. These procedures are used by manufacturers to calculate SAR for their MRI systems. Two basic methods are permitted: 1) pulse-energy method and 2) calorimetric method.
In the Pulse Energy Method a directional coupler is used to measure forward and reflected power together with an oscilloscope to measure peak-to-peak voltages. Coil losses are assessed using a non-loading phantom, while a loading phantom is used to measure sample losses. In the Calorimetric Method an insulated loading phantom is used with direct measurement of temperature. From the degree of temperature increase the absorbed energy and SAR can be computed.
Adair ER, Black DR. Thermoregulatory responses to RF energy absorption. Bioelectromagnetics 2003; 24(S6):S17-S38. [DOI Link]
Brink WB, van den Brink, Webb AG. The effect of high-permittivity pads on specific absorption rate in radio frequency-shimmed dual-transmit cardiovascular magnetic resonance at 3T. J Cardiovasc Magn Reson 2015; 17:82. [DOI link]
Collins CM, Wang Z. Calculation of radiofrequency electromagnetic fields and their effects in MRI of human subjects. Magn Reson Med 2011; 65:1470-1482. [DOI link]
Chou CK, Bassen H, Osepchuk J, et al. Radio frequency electromagnetic exposure: tutorial review on experimental dosimetry. Bioelectromagnetics 1996; 17:195-208. [DOI link]
Foster KR, Glaser R. Thermal mechanisms of interaction of radio frequency energy with biological systems with relevance to exposure guidelines. Health Phys 2007; 92:609-620. [DOI link]
International Electrotechnical Commission. IEC 60601-2-33:2010: Medical Electrical Equipment - Part 2-33: Particular Requirements for the Basic Safety and Essential Performance of Magnetic Resonance Equipment for Medical Diagnosis. 3rd ed. with amendments. International Electrotechnical Commission; 2015. (accessed September 2020)
National Electrical Manufacturers Association. NEMA Standards Publication MS 8-2016. Characterization of the Specific Absorption Rate (SAR) for Magnetic Resonance Imaging Systems.NEMA, Washington, DC. Can be downloaded for free or purchased in book form here.
Panych LP, Madore B. The physics of MRI safety. J Magn Reson Imaging 2018; 47:28-43. [DOI link]
Royal Academy of Engineering. The study of Root Mean Square (RMS) value. Available from www.stem.org.uk at this link. (provides derivation of the RMS equation as it applies to sinusoidal currents).
What practical steps can a technologist use to reduce SAR?
How do radiofrequency fields affect biological tissues?
What are the absolute SAR limits you are not permitted to exceed?